Hypothyroidism and Pregnancy:

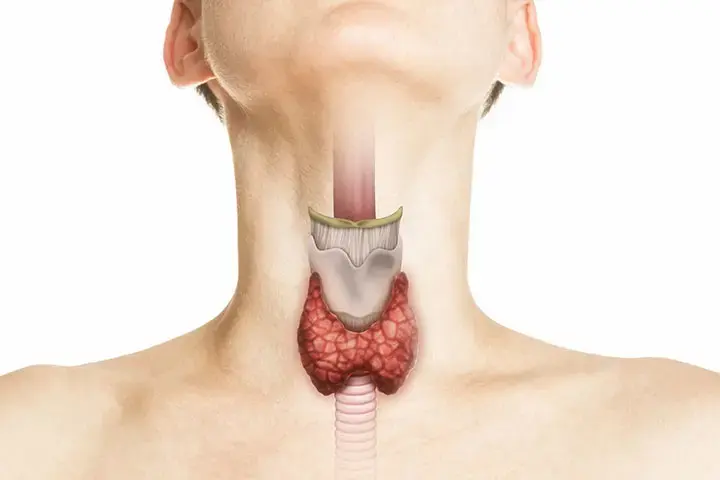
The thyroid gland, though small, plays a crucial role in maintaining overall health. Located in the neck and measuring about 2 inches (5 centimeters) across, it comprises two lobes connected by an isthmus. Typically, the thyroid is not visible and is barely palpable. However, when enlarged, it may become noticeable, leading to a condition known as a goiter, which appears as a bulge in the neck, sometimes below or beside the Adam’s apple. The thyroid produces hormones essential for regulating the body’s metabolic rate, stimulating protein production, and increasing cellular oxygen use. These hormones significantly impact heart rate, calorie burning, skin maintenance, growth, heat production, fertility, and digestion.
Locating the Thyroid Gland and Its Changes with Aging
The thyroid gland is situated in the neck and may gradually shift lower with age. Aging can cause the gland to shrink slightly, with a potential minor decrease in triiodothyronine (T3) levels. Despite these changes, essential functions typically remain stable. Thyroid disorders such as hyperthyroidism and hypothyroidism become more prevalent with age. These conditions can present symptoms that might be mistaken for other age-related issues. As a result, regular measurement of thyroid-stimulating hormone (TSH) levels is sometimes recommended for individuals over 70 years old, although there is debate about routine screening in asymptomatic individuals to prevent over-treatment.
Hypothyroidism Hormones and Their Regulation
Thyroid Hormones:
- T4 (Thyroxine): The primary hormone produced by the thyroid, T4, has minimal direct effect on metabolic rate and is converted into T3.
- T3 (Triiodothyronine): The more active thyroid hormone, T3, significantly increases the body’s metabolic rate. T4 is converted into T3 primarily in the liver and other tissues.
Hormone Transport and Activity:
Most T4 and T3 circulate in the bloodstream bound to a protein called thyroxine-binding globulin. Only the free (unbound) hormones are active. When free hormones are utilized, some of the bound hormones are released from their binding protein.
Iodine and Hormone Production:
Iodine, sourced from food and water, is essential for the production of thyroid hormones. The thyroid gland traps iodine and processes it into hormones. Excessive iodine in the blood results in a slight reduction in hormone release.
Calcitonin:
In addition to thyroid hormones, the thyroid gland produces calcitonin, which helps in strengthening bones by assisting in calcium incorporation.
Regulation of Thyroid Hormones:
The hypothalamus releases thyrotropin-releasing hormone, prompting the pituitary gland to produce thyroid-stimulating hormone (TSH). TSH then stimulates the thyroid gland to produce thyroid hormones. The pituitary gland adjusts TSH levels based on the thyroid hormone concentrations in the blood.
Diagnostic Tests of the Thyroid Gland
Physical Examination:
Doctors assess the neck to detect any enlargement or nodules in the thyroid gland.
Thyroid Function Blood Tests:
- TSH (Thyroid-Stimulating Hormone)
- T4 (Thyroxine)
- T3 (Triiodothyronine)
These tests evaluate how well the thyroid gland is functioning.
Thyroid Function Testing and Diagnostic Procedures:
TSH Testing:
TSH levels are the primary indicator of thyroid function. Elevated TSH suggests hypothyroidism, while low TSH indicates hyperthyroidism. For individuals on thyroid hormone medication, TSH levels are monitored regularly to adjust dosages.

Thyroid Hormone Testing:
Both total and free forms of T4 and T3 are measured. Free T4 and free T3 represent the active forms of these hormones. Thyroxine-binding globulin levels can affect the interpretation of total hormone levels, influenced by factors such as kidney disease, liver disease, and pregnancy.
Thyroid Ultrasound:
Used to evaluate thyroid nodules, this test assesses gland size and whether nodules are solid or cystic.
Radioactive Iodine Uptake Test:
A small amount of radioactive iodine or technetium is injected, and a gamma camera captures images of the thyroid gland. This test helps determine the activity levels of specific areas of the thyroid.
Thyroid Antibodies Test:
Performed when an autoimmune disorder is suspected, this test detects antibodies attacking the thyroid gland.
Thyroid Biopsy:
A needle biopsy of thyroid tissue is conducted if thyroid cancer is suspected, often guided by ultrasound.
Calcitonin Test:
Measured if medullary thyroid cancer is suspected, as these cancers secrete calcitonin.
Thyroid Disease: Screening and Pregnancy Implications
Screening for Thyroid Disorders:
Some experts suggest screening individuals over 70 years old for thyroid disease by measuring TSH levels. However, many medical societies advise against screening asymptomatic adults to avoid over-treatment. Newborns are routinely screened for congenital hypothyroidism to prevent severe developmental defects.
Thyroid Disease in Pregnancy:
Thyroid disease is the second most common endocrine disorder during pregnancy, following diabetes. Pregnancy increases the thyroid gland’s size by about 10% in iodine-sufficient areas and up to 40% in iodine-deficient regions. Thyroid hormone production increases by approximately 50% during pregnancy, accompanied by a similar rise in iodine requirements. Thyroid dysfunction, including hypothyroidism and hyperthyroidism, requires careful monitoring and treatment during pregnancy. Additionally, thyroid nodules and thyroid cancer may present unique challenges and may need further intervention.
Hypothyroidism Disease in Pregnancy
Etiology:
- Hypothyroidism:
- Common Causes: Chronic Autoimmune Thyroiditis (Hashimoto Thyroiditis) and endemic iodine deficiency.
- Hyperthyroidism:
- Common Causes: Graves Disease and less common conditions like toxic multinodular goiter, toxic adenoma, thyroiditis, and transient gestational thyrotoxicosis.
Epidemiology:
- Hypothyroidism: Occurs in about 2% to 3% of pregnancies, with overt hypothyroidism affecting 0.3% to 0.5% and subclinical hypothyroidism affecting 2% to 2.5%.
- Hyperthyroidism: Affects up to 0.1% to 0.4% of pregnancies.

Pathophysiology:
Normal thyroid physiology during pregnancy involves increased metabolic needs, leading to elevated serum thyroxine-binding globulin (TBG) and higher total T4 and T3 levels. hCG stimulation during pregnancy decreases serum TSH levels.
Thyroid Function and Iodine Requirements During Pregnancy
Trimester-Specific TSH Ranges:
TSH levels are monitored carefully throughout pregnancy to ensure they remain within trimester-specific ranges. If these ranges are not available, guidelines suggest adjusting the TSH reference limits accordingly.
Iodine Requirements:
Pregnancy increases iodine demand due to higher maternal thyroid hormone production and fetal iodine needs. Recommendations include 250 mcg of iodine daily during pregnancy and lactation. Excessive iodine intake should be avoided to prevent fetal hypothyroidism and goiter.
History and Physical Examination for Thyroid Disorders in Pregnancy
Hypothyroidism:
- Symptoms: Fatigue, constipation, weight gain, cold intolerance.
- Physical Examination Findings: Dry skin, puffy face, periorbital edema, delayed relaxation of deep tendon reflexes, bradycardia.
Hyperthyroidism:
- Symptoms: Palpitations, excessive sweating, heat intolerance, anxiety, insomnia, weight loss, tremors.
- Physical Examination Findings: Tachycardia, lid lag, diaphoresis, hyperreflexia. Graves Disease may present with diffuse goiter, ophthalmopathy, and pretibial myxedema.
Evaluation of Thyroid Disorders in Pregnancy:
Hypothyroidism is defined by elevated TSH levels, while hyperthyroidism is characterized by decreased TSH and increased free T4 levels. Subclinical forms of these disorders are also identified based on thyroid function tests.
Treatment and Management of Thyroid Disorders During Pregnancy
Hypothyroidism:
- Overt Hypothyroidism: Requires thyroid hormone replacement to maintain TSH levels within trimester-specific ranges. Monitoring is crucial throughout pregnancy, with dosage adjustments as needed.
- Subclinical Hypothyroidism: Treatment is recommended for women with positive TPO antibodies and elevated TSH levels. Regular monitoring is essential.
Hyperthyroidism:
- General Management: The goal is to maintain mild maternal hyperthyroidism while preventing fetal hypothyroidism. Antithyroid drugs, beta-blockers, and in rare cases, surgery, are used based on the condition’s severity and etiology.
Differential Diagnosis:
The differential diagnosis for thyroid disorders during pregnancy mirrors that of non-pregnant individuals. Thyroid nodules and cancer evaluations follow similar protocols, with specific considerations for safety during pregnancy.
Complications:
- Hypothyroidism: Untreated hypothyroidism can lead to preterm labor, preeclampsia, low birth weight, and neuropsychological impairment in the fetus.
- Hyperthyroidism: Untreated hyperthyroidism may result in preterm labor, intrauterine growth restriction, stillbirth, and fetal malformations.
Thyroid Antibodies in Euthyroid Pregnant Women:
Women with thyroid peroxidase antibodies (TPO Ab) are at higher risk of developing hypothyroidism. While there is no conclusive evidence supporting routine levothyroxine supplementation for euthyroid women with TPO Ab positivity, a small dose may be considered for those with a history of miscarriage.

